Digoxin
Digoxin
- In our pharmacy, you can buy digoxin without a prescription, with delivery in 5–14 days throughout the United Kingdom. Discreet and anonymous packaging.
- Digoxin is intended for the treatment of heart failure and atrial fibrillation. The drug is a cardiac glycoside that increases the force of heart contractions.
- The usual dose of digoxin for heart failure is 0.125–0.25 mg daily, and for atrial fibrillation, it is usually 0.25 mg daily.
- The form of administration is a tablet, capsule, oral solution, or injectable.
- The effect of the medication begins within 1 to 2 hours for oral forms and within minutes for injectable forms.
- The duration of action is typically 24 to 36 hours.
- It is advised to avoid alcohol consumption while taking digoxin.
- The most common side effect is nausea.
- Would you like to try digoxin without a prescription?
Basic Digoxin Information
- Inn (International Nonproprietary Name): Digoxin
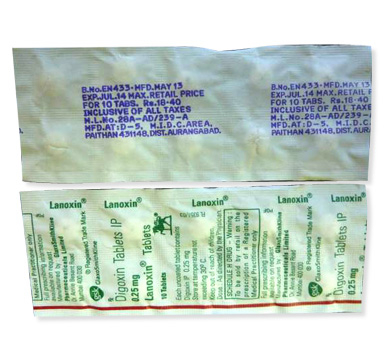
- Brand Names Available in United Kingdom: Lanoxin, Digitek, and others
- ATC Code: C01AA05
- Forms & Dosages: Tablets (0.0625 mg, 0.125 mg, 0.25 mg), injections
- Manufacturers in United Kingdom: Pfizer, Mylan, Sandoz
- Registration Status in United Kingdom: Prescription only
- OTC / Rx Classification: Prescription-only (Rx)
Everyday Use & Best Practices
For those on digoxin, establishing a consistent daily routine is crucial to ensure optimal therapeutic effects and maintain steady drug levels in the bloodstream. Patients can choose to take their dose either in the morning or the evening. Keeping to the same time each day is essential. For individuals prone to experiencing side effects such as dizziness, evening dosing may offer advantages, as this timing affords them the chance to rest through any initial adverse reactions.
When it comes to meals, digoxin can be taken independent of food; however, consistency is key. For those who choose to take it with meals, sticking to the same routine is recommended to avoid fluctuations in how the body absorbs the medication. Notably, the typical UK diet often includes high-fibre foods, which may bind with medications, potentially impairing effectiveness. It’s wise to avoid excessively high-fat meals as these may also negatively impact absorption.
Safety Priorities
While digoxin can be a lifeline for many patients, there are specific groups for whom it is not suitable. The Medicines and Healthcare products Regulatory Agency (MHRA) warns that those with conditions such as ventricular fibrillation, or those with hypersensitivity to digitalis glycosides, should steer clear of digoxin. Caution is also advised for individuals with renal impairment, electrolyte imbalances, and various arrhythmias due to the increased risk of serious side effects.
Patients should also be mindful of the potential side effects associated with digoxin, which include dizziness and fatigue. These can affect activities requiring full attention, such as driving or operating machinery. Until a patient’s response to the medication is well understood and assessed by a healthcare professional, it’s advisable to limit or avoid such tasks.
Dosage & Adjustments
According to NHS guidance, the standard initial dosage of digoxin for treating heart failure ranges from 0.125 to 0.25 mg daily. However, dosage may need adjustments based on the patient’s response to the drug, and levels should be monitored through regular blood tests. Older adults often require lower doses due to reduced renal function, necessitating careful monitoring to avoid toxicity.
In special circumstances, such as in children, dosages are typically calculated based on weight. For those with hepatic impairment, close monitoring is essential to prevent complications. Additionally, any adjustments must take into account other medical conditions or co-existing health issues.
User Testimonials
Numerous UK patients have shared their positive experiences with digoxin, particularly in managing heart failure and atrial fibrillation. Many report a noticeable improvement in their energy levels and a marked reduction in symptoms, indicating that digoxin plays a critical role in their treatment regimen.
However, it is important to highlight that not all experiences are wholly positive. Several patients have expressed their difficulties in managing side effects or adapting to the medication schedule. Concerns about potential toxicity are frequently echoes in online forums like Patient.info, where discussions around digoxin often highlight the necessity for ongoing education and support.
Buying Guide
When considering how to buy digoxin in the UK, it's important to know where to source it safely. Major pharmacy chains like Boots, LloydsPharmacy, and Superdrug offer digoxin, either through prescription or via NHS services. For optimal safety, always ensure prescriptions are filled at trusted pharmacies.
Cost is a crucial factor to keep in mind. NHS prescription charges currently stand at £9.35 in England, yet other regions like Scotland, Wales, and Northern Ireland provide prescribed medications free of charge. For those looking into private options, prices may vary considerably, potentially resulting in higher costs. Researching options upfront can save money in the long run.
What’s Inside & How It Works
The primary active ingredient in digoxin is digoxin itself, along with various excipients that aid in absorption and enhance stability. Patients can find it in different strengths, typically 0.0625 mg, 0.125 mg, and 0.25 mg tablets, catering to diverse patient needs.
So, how does digoxin work? By inhibiting the Na+/K+ ATPase pump, it increases intracellular calcium, which enhances heart contractility. This action significantly benefits patients dealing with heart failure or atrial fibrillation, as it boosts cardiac output and can help manage symptoms effectively.
Main Indications
Digoxin has received approval for various indications and is particularly effective in managing heart failure and atrial fibrillation. The MHRA recognises its ability to enhance heart function, especially in patients who still experience symptoms despite undergoing other treatments.
Beyond its approved uses, digoxin may also be prescribed off-label in UK clinics for specific arrhythmias, particularly in paediatric patients suffering from congenital heart disease. This demonstrates the versatility of digoxin, allowing healthcare practitioners to tailor treatment based on individual clinical needs.
Interaction Warnings
Food interactions are a concern for patients on digoxin. It's crucial to avoid excessive alcohol consumption, as it can heighten side effects like dizziness. Additionally, strong teas and coffee can impede the absorption of digoxin, so timing its intake around meals and beverages needs careful consideration.
When it comes to drug interactions, particular caution is warranted. Medications such as amiodarone, verapamil, and certain antibiotics may elevate digoxin levels in the bloodstream, raising the risk of toxicity. Patients should always discuss any concurrent medications with their healthcare provider or pharmacist to identify potential conflicts, thereby ensuring both safety and efficacy.
Latest Evidence & Insights
Recent studies conducted in the UK and EU from 2022 to 2025 underscore the ongoing importance of digoxin in managing conditions like heart failure and atrial fibrillation. Research efforts are increasingly focusing on optimising dosing protocols and monitoring strategies. The aim is to reduce the risk of digoxin toxicity while enhancing patient outcomes. These studies reiterate a critical point: careful management of digoxin is essential, as it maintains a narrow therapeutic index. Intense scrutiny on dosing adjustments helps mitigate any potentially severe side effects related to digoxin use. The body of evidence shows that patients can experience significant improvements when digoxin therapy is tailored to their specific circumstances. Notably, researchers are emphasising the need for regular blood level monitoring, particularly in patients with renal impairment. Thus, digoxin continues to be a cornerstone in cardiac care, allowing healthcare providers to offer more targeted treatments for individuals. The findings fuel ongoing discussions within the medical community regarding evidence-based approaches to digoxin usage, reshaping discussions aimed at increasing awareness of risks and benefits effectively.Alternative Choices
In the realm of alternative medications, several options are available for patients who may require substitutes for digoxin, particularly within the NHS framework. Options such as beta-blockers and ACE inhibitors are commonly considered due to their diverse effects on cardiac function. Here’s a brief pros and cons checklist for some alternatives: - **Beta-Blockers**: - **Pros**: Reduce heart rate; beneficial for hypertension and heart failure. - **Cons**: May cause fatigue and could lower heart rate excessively. - **ACE Inhibitors**: - **Pros**: Excellent for controlling blood pressure; more optimal renal outcomes. - **Cons**: Risk of cough and possible renal function decline. Deciding on an alternative necessitates a careful evaluation of the patient's overall health status, specific cardiac needs, and potential for adverse effects associated with these medications. Ultimately, healthcare professionals play a crucial role in ensuring that the selected alternative aligns with the patient’s treatment goals and overall therapy efficacy.Regulation Snapshot
The prescription framework for digoxin within the UK is overseen meticulously by the Medicines and Healthcare products Regulatory Agency (MHRA). Their stringent guidelines govern how digoxin is prescribed and monitored, ensuring safety and efficacy throughout therapy. Healthcare providers are required to follow these guidelines to tailor therapies according to individual patient health needs. Monitoring protocols emphasise regular blood testing to maintain appropriate therapeutic levels and detect any signs of toxicity early. Moreover, ongoing education on guidelines ensures healthcare professionals remain vigilant regarding the risks associated with digoxin, particularly considering its complex interaction with other medications. Compliance with MHRA regulations is paramount for safeguarding patient health and optimising treatment outcomes in cardiac care.FAQ Section
1. **Can digoxin cause death?** Rarely, but overdose or significant drug interactions can be lethal, making regular monitoring essential. 2. **Is digoxin a blood thinner?** No, it does not act as a blood thinner but plays a critical role in controlling heart rhythm. 3. **How often should digoxin levels be checked?** Regular monitoring is vital, typically every 6–12 months, but more frequently if any concerns arise about toxicity or patient health status. These common questions reflect the importance of understanding digoxin use and its implications. Access to accurate information helps patients manage their care effectively and highlights the need for ongoing discussions with healthcare providers about treatment options.Guidelines for Proper Use
Consulting pharmacists is vital for patients who are prescribed digoxin. They can provide insights on dosages, what patients should expect during therapy, and how to manage potential adverse effects. This professional guidance is crucial for understanding how to administer digoxin safely. The NHS also offers comprehensive support resources for ongoing patient education surrounding digoxin. These include: - **Dosage schedules**: Ensuring patients adhere to their prescribed regimens. - **Dietary advice**: Understanding foods that may interact with the medication. - **Importance of adherence**: Stressing the need for consistent use to promote optimal outcomes. Such resources not only aid patients but also empower healthcare providers to deliver informed counselling, fostering better health management.| City | Region | Delivery Time |
|---|---|---|
| London | Greater London | 5–7 days |
| Birmingham | West Midlands | 5–7 days |
| Manchester | Greater Manchester | 5–7 days |
| Glasgow | Scotland | 5–7 days |
| Newcastle | Tyne and Wear | 5–7 days |
| Leeds | West Yorkshire | 5–7 days |
| Cardiff | Wales | 5–7 days |
| Bristol | South West England | 5–7 days |
| Sheffield | South Yorkshire | 5–7 days |
| Nottingham | East Midlands | 5–9 days |
| Leicester | East Midlands | 5–9 days |
| Coventry | West Midlands | 5–9 days |
| Hull | East Yorkshire | 5–9 days |
| Stoke-on-Trent | Staffordshire | 5–9 days |